Abstract

Diffuse large B-cell lymphoma (DLBCL) is the most common type of B-cell lymphoma in the United States. The introduction of rituximab has significantly improved outcomes in the treatment of DLBCL. However, relapsed and refractory cases still pose a challenge. More recently, our understanding of the biology of DLBCL has evolved such that assessment of molecular risk through evaluation of the cell of origin and specific genetic mutations are being incorporated into prognostication and treatment decisions. The location of extranodal involvement has been implicated in the prognosis, but the prognostic relevance of the location of lymphadenopathy has not been extensively investigated.
Methods
We used the Surveillance, Epidemiology, and End Results (SEER) database to extract cases of nodal DLBCL from 1983 to 2014. The SEER database considers spleen and Waldeyer's Ring (WR) as nodal, so they were included in the extraction. A total of 71,132 cases were identified. Cases without follow-up, with unknown Ann-Arbor stage (extranodal involvement is not included in the database), with more than one primary tumor, without histologic confirmation of the disease, and with an unspecified location or lymph nodes in multiple regions, were excluded. Age was categorized into the following groups: 20-39,40-59, 60-75, and >75 years. Treatment characteristics for included patients were extracted and cases were dichotomized based on the year of diagnosis; 2000 was used as a cut-off because the first landmark study evaluating R-CHOP was presented at the American Society of Hematology (ASH) meeting in December of that year. Survival curves were estimated by the Kaplan-Meier method and were compared using the log-rank test. A Cox proportional hazard model was constructed to identify the hazard ratios (HR) for each location. ANOVA was used to adjust for age, stage, gender, race, year of diagnosis, administration of chemotherapy, administration of radiation, and cancer-directed surgery. A chi-square test was utilized to compare categorical variables. Proportionality was tested with Schoenfeld residuals. Statistical analysis was performed with R statistics.
Results
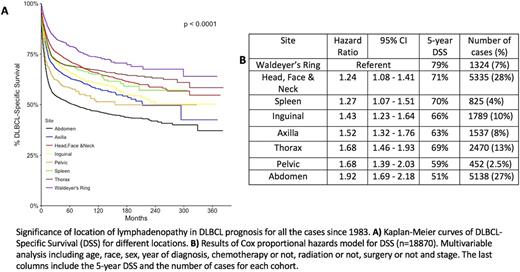
A total of 18,870 cases were included in the analysis. The majority of these cases were located in the head/face neck (28%) and abdomen/retroperitoneum (27%).The overall 5-year DLBCL-specific survival (DSS) was 65%. The location of lymphadenopathy was predictive of outcome after adjusting for all other factors (p<.001). In the total cohort, involvement of WR was associated with better survival (79%) and involvement of the abdomen with the poorest survival (51%). Similar results were produced by the Cox model with WR having the best survival (referent) whereas the abdomen had the worst (hazard ratio 1.92, 95% CI 1.69-2.18). When comparing the pre-rituximab and post-rituximab data, the survival of patients from all locations improved, apart from patients who had pelvic lymphadenopathy (HR 0.77, 95% CI 0.55-1.08, p= 0.12). WR and abdomen retained the best and the worst survival, respectively, in both eras. Kaplan-Meier curves for all cases since 1983 are presented in Figure A, whereas the results of the Cox model are presented in Table B . Patients who were diagnosed with DLBCL in the thorax were much younger than all other patients combined (39% vs 8% in 20-39 years, p < .001).
Conclusions
This is the first large study demonstrating a statistically significant difference in survival for patients with nodal DLBCL depending on the primary location of their disease. One possible explanation is that patients with intrathoracic or intraabdominal disease are more vulnerable to vital organ compromise. WR cases probably include cases of large B-cell lymphoma with IRF4 rearrangement, which have a better prognosis. In addition, primary mediastinal B-cell lymphoma was a separate entity in SEER after 2001, so many cases of thoracic DLBCL prior to that date could actually be the former. Further investigation and validation in other cohorts incorporating molecular studies is warranted before this information can be incorporated into prognostic tools.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal